The Vitamin A and D Conundrum
by Alden Ryno on March 20, 2015The Vitamin A and D Conundrum
The fact that you’re reading this on the Mountain Dog site means that you probably take a variety of vitamins and supplements throughout the day. You likely have specific reasons why you take some of them while others are thrown in because “you should” take them or they are along for the ride with your multivitamin. A vitamin that has really gained momentum in past years is Vitamin D, and for great reasons! Vitamin D participates in numerous bodily functions ranging from bone growth and health to protecting against depression and promoting proper β-cell function which results in enhanced insulin sensitivity.1-4 Despite decades of research concerning the functions of vitamin D research, there are still profound benefits being discovered today. In fact, Rhonda Patrick and Bruce Ames recently published data in February of 2015 showing a causal link between proper levels of Vitamin D and serotonin production affecting the development of autism in children.5,6 However, in our supplement crazed society, we are more concerned with the individual actions of one supplement rather than the interactions between distinct nutrients. Just like pharmaceutical drug interactions, we should be keenly aware of how the vitamins and supplements we ingest interact with one another. Here, we’ll take a look at vitamin A and vitamin D alone, and then in tandem in order to see what may happen between them and why we should care.
Our Essential Friends
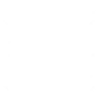
Vitamin D comes in two primary forms: Vitamin D2 (ergocalciferol) and Vitamin D3 (cholecalciferol). Cholecalciferol is the form which is found in animal tissue and is synthesized in our skin through direct sunlight from provitamin D (7-dehydrocholesterol). Ergocalciferol is the plant-based form of Vitamin D. Throughout the body, both D2 and D3 are treated quite similarly, though D3 is more easily converted to active forms of Vitamin D in the body.7
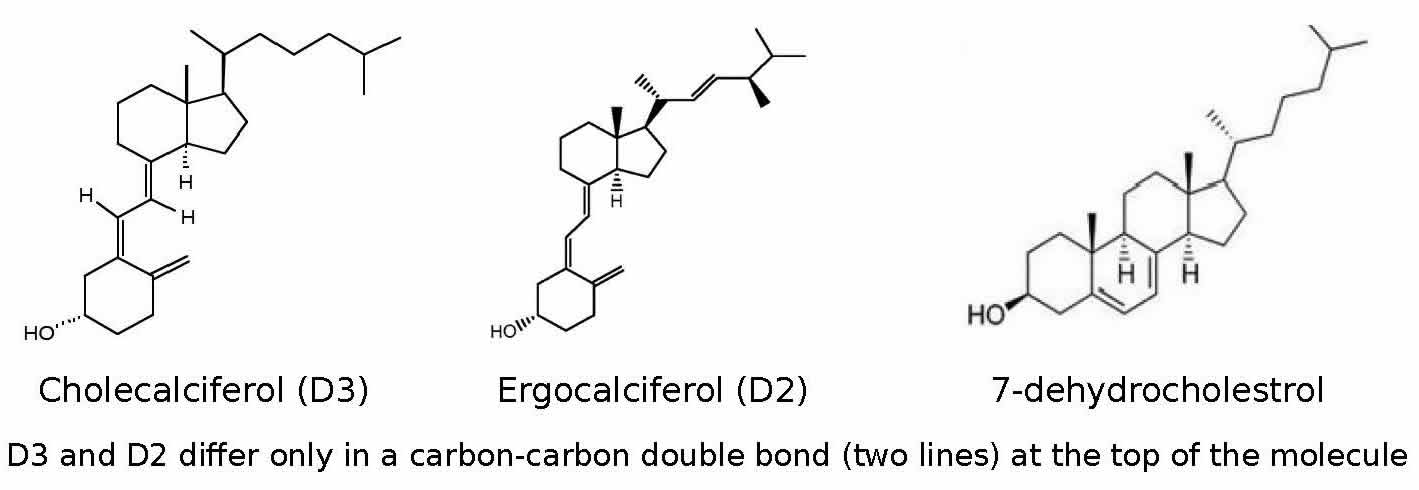
Vitamin D is absorbed in the jejunum and ileum portions of the small intestines via passive diffusion.8 Like many other vitamins, our bodies don’t use the ingested versions of Vitamin D, but converts the two into the active form(s) of Vitamin D, 1,25-dihydroxyvitamin D, or calcitriol, through two enzymatic hydroxylations in the liver and then the kidneys.9,10 Calcitriol then travels throughout the blood stream bound to Vitamin D binding proteins (VBP) where it travels to the parathyroid or various other Vitamin D Receptor (VDR) sites, which are still under investigation.11-13 Vitamin D acts as a hormone (signaling molecule) throughout the body and is a vital regulator in nutrient absorption during digestion and in calcium and phosphate concentrations in bones through restriction of the parathyroid to produce parathyroid hormone (PTH).12,14 When serum levels of Vitamin D are low, the body is signaled to pull calcium from the bones and into the blood stream due to high levels of PTH. This results in acute hypercalcemia in the blood and may lead to kidney stones.12,16 This may also result in osteoporosis if unaddressed over a long period of time.
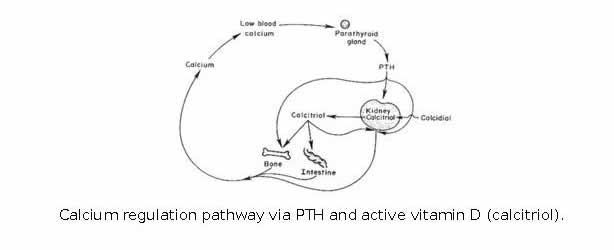
A diet rich in orange plant-based foods will almost certainly provide adequate amounts of vitamin A in the form of provitamin A, or carotenoids (β-carotene, β-cryptoxanthin, etc). These compounds are poorly converted into various types of active and preformed vitamin A (retinol, retinyl esters, and retinoic acid).16 Animal sources such as liver provide much more potent and active quantities of vitamin A. It’s unlikely that you don’t get enough vitamin A from your diet and a multivitamin, since a MV generally supplements with the active molecules of vitamin A. 16,17 Like vitamin D, vitamin A is absorbed via lipophilic micelles in the small intestine, however, it is thought that Vitamin A is absorbed via facilitated diffusion.18
So what does vitamin A do? It is essential in proper retina function in the eye; hence the name retinol. It is also a largely responsible for the growth and differentiation of epithelial cells which make up the linings of cavities in the body from the intestines to the lunges and even the eyes.16,19 A third, but lesser researched function associated with vitamin A is insulin resistance. As the transporter of vitamin A (retinol binding protein [RBP]) rises, there is a decrease in glucose transporter type 4 (GLUT4) activity and insulin sensitivity.21 These three functions, though not the only factors, clearly demonstrate the significance of vitamin A. A select few of the symptoms of hypervitaminosis A (HVA) include bone fragility, potential liver distress and disease, and increased insulin resistance.16,20,21
Who beats whom?
Interestingly enough, the first and last of those symptoms are opposites of sufficient amounts of Vitamin D. Is there an interaction between these two fat-soluble vitamins? You betcha!
The antagonistic relationship between vitamins A and D has been intriguing scientists as early as 1985 when researchers at the University of Minnesota looked into the skeletal development of turkeys. Metz, et al, found that a diet high in vitamin A and normal in vitamin D exhibited symptoms of HVA (depressed growth, impaired mobility, and weak bones) while a diet normal in vitamin A and high in vitamin D displayed only mild symptoms of heightened levels of serum vitamin D (25-hydroxycholecalciferol) such as kidney stones from elevated calcium levels.22 However, turkeys fed a diet high in both vitamins A and D were similar to turkeys fed a control diet with normal levels of vitamins A and D. This tells us that there is a point at which the vitamins essentially nullify the effects of each other. Why is that? And what are the optimal intakes for each vitamin in order to benefit from both?
We discussed that both vitamin A and D are absorbed in the small intestine and there does not appear to be any evidence to support that the vitamins interfere with one another at this level, especially since they are absorbed through different means. Let’s dig deeper into the body to see what is happening.
Once converted to their active forms via enzymes from the same family of enzymes, cytochrome P450, they bind to specific protein-based receptor sites. Vitamin A binds to retinoic acid receptors (RARs) and retinoid X receptors (RXRs); the “X” refers to any number of retinol analogs including retinoic acid, retinal, retinol, and retinyl esters. 23,24 Vitamin D binds to vitamin D receptors (VDRs) and retinoid X receptors (RXRs). We can already see that both vitamins share a common receptor in the RXRs. However, the location on the RXRs where each vitamin binds are different, and with distinct affinities (how tightly they bind).25
While vitamin D can perform many of its actions by only binding to VBPs in the blood, several other functions require a heterodimer between VDRs and RXRs in order for gene expression to occur.23,24 This is where vitamin A begins to cause problems with the actions of vitamin D. As the name suggests, retinoid X receptors preferentially bind to vitamin A analogs compared to vitamin D by more than 2 orders of magnitude. This means that when surplus vitamin A is present, it decreases the number of receptors available for vitamin D. Even though vitamin A and vitamin D bind to different locations on the receptors, the action of binding to one alters the shape of the receptor; inhibiting the binding of other molecules. This is known as allosteric competitive inhibition. While vitamin D can bind to VDRs in the presence of excess vitamin A, it is impossible for gene expression to occur without the dimeric duo of vitamin D bound VDRs and RXRs. As a result, the vitamin D-VDR complexes are metabolized and discarded before any free RXRs are available to bind.
Take note that this occurs only in the presence of excess vitamin A. It appears that there are plenty of RXRs to satisfy both vitamin A and vitamin D when levels of vitamin A are not elevated. However, the previous inhibitory mechanism may be partially overridden with an ample amount of vitamin D and vitamin A, despite the fact that vitamin A preferentially binds to the RXRs.
The previous paragraph tells us that a diet with normal levels of vitamin A and high amounts of vitamin D will produce the benefits of both vitamins. Meanwhile, a diet normal in both or high in vitamin A will negate many of the positive effects of vitamin D. As a result, it is recommended that a diet should be supplemented with vitamin D, but not so for vitamin A. This is assuming that the diet has enough foods containing carotenoids (orange foods). If not, then small amounts of vitamin A should be supplemented, preferably in the form of beta-carotene, not retinol and its analogs.16
How to Get the Best of Both Worlds
According to the NIH, the RDA for vitamin A in the form of retinol is 900 IU (equal to 900 RE [retinol equivalents] or 900 mcg retinol) and roughly 10,000-20,000 IU from β-carotene or β-cryptoxanthin. The RDA varies greatly due to the wide range of conversion from plants to retinol in the body; anywhere from 12:1 to 24:1, depending on the carotenoid source.16 For example, a normal sweet potato (~8oz/227g) provides nearly 28,000 IU of vitamin A from beta-carotene (2,300 RE). A proper diet should supply sufficient amounts of Vitamin A and supplementation further is not recommended, if you seek the benefits of supplemental vitamin D. Vitamin D, on the other hand, is hard to get from the diet, but is bountiful with 20-30 minutes of unprotected exposure to the sun, in the summer months. The RDA for vitamin D is quite low at a meager 200-600 IU for 19-50 year old adults.7 Despite that, recent research, including that of Dr. Rhonda Patrick, have warranted a significant rise in the RDA. Dr. Patrick has proposed intakes as great as 40 IU/lb (88 IU/kg or 1000 IU/25 lbs) of bodyweight for average weight adults. Her recommendations indicate an intake of up to 9,000 IU for a 225 pound male. She still recommends getting blood work done prior to such rigorous supplementation though. Optimal levels of serum vitamin D (25-dihydroxy-vitamin D) fall in the range of 20 ng/mL or 50 nmol/mL, but remain lower than 50 ng/mL or 125 ng/mL.7
To recap, we should be getting both vitamin A and D in our diet. However, we should also supplement with vitamin D (up to 1,000 IU per 25 pounds of bodyweight), especially during the winter months or when your exposure to direct sunlight is limited. I don’t believe that supplementing with vitamin A is necessary with proper diet and is even detrimental to effectively using supplemental vitamin D. If you do eat a lot of vitamin A rich foods (liver, sweet potatoes/yams, carrots, pumpkin, dark greens), then it is also advised to supplement with vitamin D in order to provide the body with plenty due to the antagonistic nature of vitamin A.
As our interests in our personal health continue to rise, we should aim to learn more about what we’re putting into our bodies. Only two nutrients were covered here while you (probably) take in dozens a day. Do you think that those other things aren’t interacting with one another? I’ll tell you now that they are. Not unlike pharmaceutical drugs, we should at least be cognizant of both antagonistic and synergistic interactions between vitamins, minerals, and any number of other supplements that we ingest. I hope that you gained a small insight into what you put into your body and you’ll be interested to learn and educate yourself further in the future.
References
- Cranney A, Horsley T, O’Donnell S, Weiler H, Puil L, Ooi D, Atkinson S, Ward L, Moher D, Hanley D, Fang M, Yazdi F, Garritty C, Sampson M, Barrowman N, Tsertsvadze A, Mamaladze V (August 2007). “Effectiveness and safety of vitamin D in relation to bone health”. Evidence report/technology assessment (158): 1–235. PMID 18088161.
- Shaffer JA, Edmondson D, Wasson LT, Falzon L, Homma K, Ezeokoli N, Li P, Davidson KW (2014).”Vitamin D Supplementation for Depressive Symptoms: A Systematic Review and Meta-Analysis of Randomized Controlled Trials”. Psychosomatic Medicine 76 (3): 190–6. doi:10.1097/psy.0000000000000044.PMID 24632894
- Kayaniyil S, Gerstein HC, Veith R, Perkins BA, Retnakaran R, Harris SB, Knight JA, Zinman B, Qi Y, H. A. (2010). Association of Vitamin D With Insulin Resistance and beta-Cell Dysfunction in Subjects at Risk for Type 2 Diabetes. Diabetes Care, 33(6), 1379–1381. doi:10.2337/dc09-2321.
- Mitri, J., Dawson-hughes, B., Hu, F. B., & Pittas, A. G. (2011). Effects of vitamin D and calcium supplementation on pancreatic b cell function , insulin sensitivity , and glycemia in adults at high risk of diabetes : the Calcium and Vitamin D for Diabetes Mellitus ( CaDDM ) randomized controlled trial 1 – 4. Am J Clin Nutr, 94(4), 486–494. doi:10.3945/ajcn.111.011684.1
- Rhonda P. Patrick, B. N. A. (n.d.). Vitamin D hormone regulates serotonin synthesis. Part 1: relevance for autism. FASEB, 28(6), 2398–2413. doi:10.1096/fj.13-246546
- Rhonda P. Patrick, B. N. A. (n.d.). Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: relevance for ADHD, bipolar, schizophrenia, and impulsive behavior. FASEB. doi:10.1096/fj.14-268342
- Gloth, F. M. (1995). Vitamin D. Lancet, 345, 1185.
- Hollander, D., Muralidhara, K. S., & Zimmerman, a. (1978). Vitamin D-3 intestinal absorption in vivo: influence of fatty acids, bile salts, and perfusate pH on absorption. Gut, 19(November 1977), 267–272. doi:10.1136/gut.19.4.267
- Blunt, J.W., DeLuca, H.F. & Schnoes, H.K. (1968). 25-hydroxycholecalciferol. A biologically active metabolite of vitamin D3. Biochem., 7: 3317-3322.
- 3. Fraser, D.R. & Kodicek, E. (1970). Unique biosynthesis by kidney of a biologically active vitamin D metabolite. Nature, 228: 764-766.
- Rochel, N., Wurtz, J. M., Mitschler, a, Klaholz, B., & Moras, D. (2000). The crystal structure of the nuclear receptor for vitamin D bound to its natural ligand. Molecular Cell, 5, 173–179. doi:10.1016/S1097-2765(00)80413-X
- Bikle, D. (2009). Nonclassic actions of vitamin D. Journal of Clinical Endocrinology and Metabolism, 94(January 2009), 26–34. doi:10.1210/jc.2008-1454
- Wang, Y., & DeLuca, H. F. (2011). Is the vitamin D receptor found in muscle? Endocrinology, 152(March), 354–363. doi:10.1210/en.2010-1109
- Jones, G., Strugnell, S. a, & DeLuca, H. F. (1998). Current understanding of the molecular actions of vitamin D. Physiological Reviews, 78(4), 1193–1231.
- Cranney A, Horsley T, O’Donnell S, Weiler H, Puil L, Ooi D, Atkinson S, Ward L, Moher D, Hanley D, Fang M, Yazdi F, Garritty C, Sampson M, Barrowman N, Tsertsvadze A, M. V. (n.d.). Effectiveness and safety of vitamin D in relation to bone health. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18088161
- Vitamin A. (n.d.). FAO/WHO Expert Consultation on Human Vitamin and Mineral Requirements, 87–107.
- Chen, W., & Chen, G. (2014). The Roles of Vitamin A in the Regulation of Carbohydrate, Lipid, and Protein Metabolism. Journal of Clinical Medicine, 3, 453–479. doi:10.3390/jcm3020453
- Dew, S.E.; Ong, D.E. (1994). Specificity of the retinol transporter of the rat small intestine brush border. Biochemistry, 33, 12340–12345.
- Ackerley, S. K. Developlmental Biology Online. “Epithelial cells”. 09 Dec 2005. 04 Sept 2010 http://www.uoguelph.ca/zoology/devobio/210labs/epithelial1.html
- Aburto, a, Edwards, H. M., & Britton, W. M. (1998). The influence of vitamin A on the utilization and amelioration of toxicity of cholecalciferol, 25-hydroxycholecalciferol, and 1,25 dihydroxycholecalciferol in young broiler chickens. Poultry Science, 77, 585–593.
- Qin Yang, Timothy E. Graham, Nimesh Mody, Frederic Preitner, Odile D. Peroni, Janice M. Zabolotny, Ko Kotani, Loredana Quadro & Barbara B. Kahn. (2005). Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature, 436, 356–362. doi:10.1038/nature03711
- Metz, a L., Walser, M. M., & Olson, W. G. (1985). The interaction of dietary vitamin A and vitamin D related to skeletal development in the turkey poult. The Journal of Nutrition, 115, 929–935.
- MacDonald, P. N., Dowd, D. R., Nakajima, S., Galligan, M. a, Reeder, M. C., Haussler, C. a, … Haussler, M. R. (1993). Retinoid X receptors stimulate and 9-cis retinoic acid inhibits 1,25-dihydroxyvitamin D3-activated expression of the rat osteocalcin gene. Molecular and Cellular Biology, 13(9), 5907–5917. doi:10.1128/MCB.13.9.5907.Updated
- Thompson, P. D., Jurutka, P. W., Haussler, C. a, Whitfield, G. K., & Haussler, M. R. (1998). Heterodimeric DNA Binding by the Vitamin D Receptor and Retinoid X Receptors Is Enhanced by 1 , 25-Dihydroxyvitamin D 3 and Inhibited by 9-cis-Retinoic Acid, 273(14), 8483–8491.
- Richard A. Heyman, David J. Mangelsdorf, Jacqueline A. Dyck, Robert B. Stein, Gregor Eichele, Ronald M. Evans, C. T. (1992). 9-cis retinoic acid is a high affinity ligand for the retinoid X receptor. Cell, 68(2), 397–406. doi:10.1016/0092-8674(92)90479-V